Cofactor AI: Revolutionizing Healthcare Revenue Cycle Management with AI-Powered Appeals
Cofactor AI is transforming the healthcare revenue cycle management (RCM) process by leveraging the power of artificial intelligence to simplify and streamline insurance appeals. The platform automates complex tasks, identifies appealable denials, and maximizes reimbursement rates, ultimately helping providers recover lost revenue and improve operational efficiency.
Key Features of Cofactor AI
- AI-Driven Denial Identification: Cofactor's AI engine analyzes millions of data points to identify appealable denials with pinpoint accuracy, ensuring no potentially recoverable revenue is missed.
- Automated Documentation Gathering: The platform automates the process of gathering necessary documentation for appeals, saving valuable time and resources.
- Streamlined Submission Formatting: Cofactor ensures all submissions adhere to payer-specific formatting requirements, minimizing rejection rates due to formatting errors.
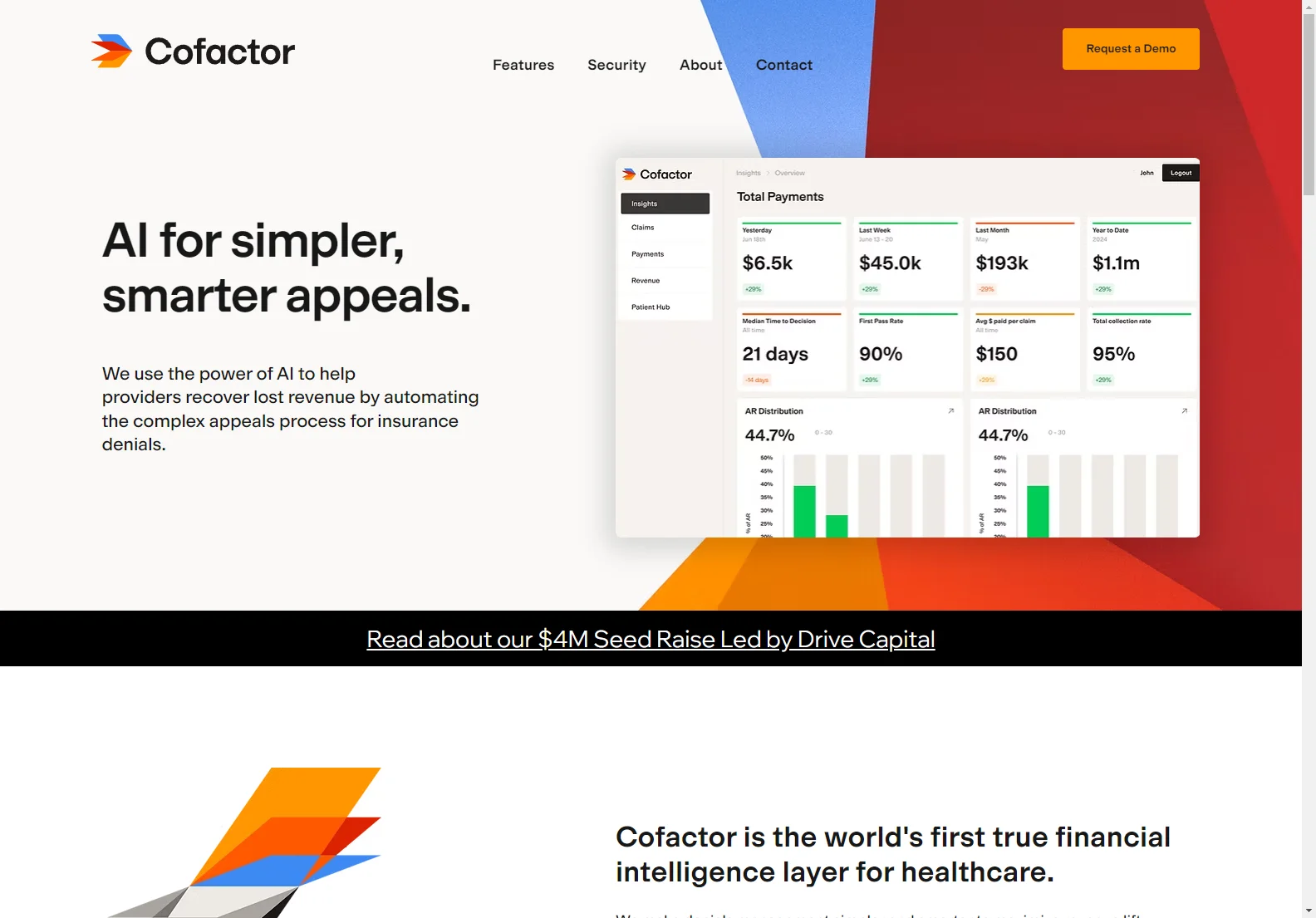
- Real-time Status Tracking: Monitor the status of all appeals in real-time, providing complete transparency and control over the process.
- Enhanced Appeal Success Rates: By leveraging AI-powered insights and identifying the precise evidence payers require, Cofactor significantly increases the likelihood of successful appeals.
- Reduced Days in A/R: Automated appeals significantly reduce the time it takes to receive reimbursements, improving cash flow and reducing days in accounts receivable.
- Lower Cost to Collect: Streamline your appeals process, freeing up your team to focus on higher-value tasks and reducing the overall cost of revenue cycle management.
How Cofactor AI Benefits Healthcare Providers
Cofactor AI offers a multitude of benefits to healthcare providers, including:
- Increased Revenue Recovery: Maximize revenue by recovering reimbursements from previously denied claims.
- Improved Operational Efficiency: Automate time-consuming tasks, freeing up staff for other critical responsibilities.
- Reduced Administrative Costs: Streamline workflows and minimize the expenses associated with manual appeals processing.
- Enhanced Cash Flow: Faster reimbursements lead to improved cash flow and financial stability.
- Data-Driven Insights: Gain valuable insights into denial trends and patterns to proactively address issues and prevent future denials.
Cofactor AI vs. Traditional Appeals Management
Traditional appeals management methods are often manual, time-consuming, and prone to errors. Cofactor AI offers a significant advantage by automating key processes, improving accuracy, and significantly increasing the efficiency of the appeals process. This leads to higher recovery rates and reduced administrative costs compared to manual processes.
Conclusion
Cofactor AI is a game-changer in healthcare revenue cycle management. By harnessing the power of AI, it empowers providers to recover lost revenue, improve efficiency, and focus on delivering high-quality patient care. Request a demo today to see how Cofactor AI can transform your RCM process.